Today’s morning report case involved a woman with a previous
history of metastatic malignancy presenting with dyspnea. She was found on imaging to have a
substantial pleural effusion as well as a substantial pericardial
effusion. We spoke about a number of
valuable learning topics:
· Whenever you are confronted with someone with a
pericardial effusion or even a patient with a condition that would predispose
to effusions, you should consider
pericardial tamponade as a diagnostic entity. Without considering it, you won’t test for it
or diagnose it!
· Conditions that predispose to effusions are:
o
Pericarditis
can produce serous or blood effusions, especially for anticoagulated patients
o
Infections
such as tuberculosis
o
Malignancies
like lung cancer, lymphoma, or any metastatic disease
o
Uremia
producing uremic pericarditis and an effusion
o
Post-myocardial
infarction pericarditis leading to an effusion
o
Conditions
leading to arterial bleeding within the pericardial sac (dissections,
iatrogenic injury, etc.)
· It is important to note that the pericardium is
a rigid structure that can become compliant with time. Therefore, malignant effusions that have as
much as 1.5L of fluid may not produce pericardial tamponade if they develop
slowly. By contrast, 30cc of arterial
blood from a coronary artery dissection immediately into a rigid pericardium
can rapidly produce tamponade.
· There are several features to find on physical
examination when we discuss pericardial tamponade:
o
From a
vital sign perspective, patients are often hypotensive. This has to do with impairment of atrial info
to both sides of the heart owing to increased pericardial pressure.
o
It is
valuable to perform a pulsus paradoxous
in this and other conditions. The pulsus
paradoxus is inaptly named because it is actually an exaggeration of a normal
phenomenon. To measure it, take a blood
pressure with auscultation – when deflating the cuff slowly, you will hear
Korotkoff sounds only on expiration beginning at a certain pressure. Note this pressure and continue – you will
then hear the sounds throughout the respiratory cycle. The difference between those two pressures is
the pulsus paradoxus. Many have
suggested that this phenomenon occurs due to reduced pulmonary vascular
resistance upon inspiration, increased venous inflow into the RA/RV, and then
septal bowing into the LV impairing LV outflow.
While this makes sense, it is not seen echocardiographically even during
tamponade. Instead, the mechanism is
thought to be related to the gradient of pressure in the pulmonary veins
(mostly affected by the intrathoracic pressure) and the left atrium (mostly
affected by pericardial pressure).
Normally, when you breathe in, your intrathoracic pressure becomes
negative meaning that there is a slight impediment to flow from pulmonary veins
to left atrium. That impediment (and the
pulsus paradoxus) becomes larger if the negative pressure in the thorax
increases (e.g. during an asthma exacerbation, COPD exacerbation, or pulmonary
embolism) or if there is an impediment to left atrial inflow (high
intrapericardial pressure). Pulsus
paradoxus does not occur (at least to
the same level) with constrictive
pericarditis because the issue there is not pressure being transmitted onto the atrium, but rather rigid pericardium that resists
stretching as soon as the heart fills.
o
Frequently
overlooked but useful according to the JAMA rational clinical exam, is
tachycardia.
o
When
examining the patient’s neck, you will often notice distended neck veins, once
again owing to obstruction of venous inflow.
o
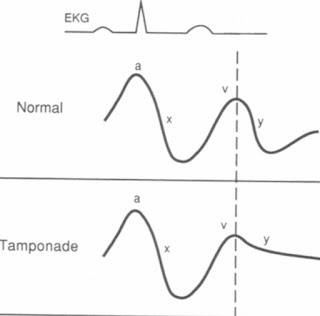
The JVP
waveform (easier to view on a central venous catheter than by eye) will usually
show a blunted y-descent which can
help distinguish tamponade from other pericardial problems. The y-descent occurs when the tricuspid valve
opens and passive filling of the ventricles begins – high pericardial pressures
inhibit right atrial and right ventricular inflow. The x-descent is still prominent in tamponade
because there is a vacuum phenomenon that occurs during ventricular systole
allowing blood to enter despite the high pericardial pressures.
o
One often
hears muffled heart sounds, but this isn’t as common as you may think.
o
On ECG,
the common findings are low voltages (usually if there is a lot of pericardial
fluid) and electrical alternans
meaning that the QRS axis changes from beat-to-beat. You can think of the heart “swinging” in the
pericardial sac.
· To treat tamponade, which is a mechanical
problem, usually a mechanical solution is required. Pericardiocentesis can be performed
percutaneously, but surgical options such as a pericardial window are also
possible. The medical management of
tamponade in the interim usually involves provision of a lot of intravenous
fluids.
· Tamponade needs to be distinguished from two
other syndromes – Constrictive
Pericarditis and Restrictive
Cardiomyopathy.
|
|
Tamponade
|
Constrictive
Pericarditis
|
Restrictive
Cardiomyopathy
|
|
Vitals
|
+++ Pulsus
paradoxus, hypotension
|
Smaller pulsus,
hypotension
|
Hypotension
|
|
JVP
|
Elevated
|
Kussmaul sign (rise
with inspiration)
|
Kussmaul sign
|
|
Apex Beat
|
Impalpable
|
Impalpable or retracting on systole
|
Palpable
|
|
Heart sounds
|
Muffled
|
Pericardial knock
|
S3 but no knock
|
|
Ventricular
Interdependence (on angiography)
|
High
|
High
|
None (e.g.
concordant respiratory changes on simultaneous RV/LV recording)
|
· It’s worth noting that there are situations
where the pulsus paradoxus is absent
despite the patient having tamponade.
The main one is a large atrial septal defect, which allows equalization
of the atrial pressures and obliterates the pulsus.
Further Reading:
Little, W. C., &
Freeman, G. L. (2006). Pericardial disease. Circulation, 113(12),
1622-1632.
Roy, C. L., Minor, M.
A., Brookhart, M. A., & Choudhry, N. K. (2007). Does this patient with a
pericardial effusion have cardiac tamponade?. JAMA, 297(16),
1810-1818.