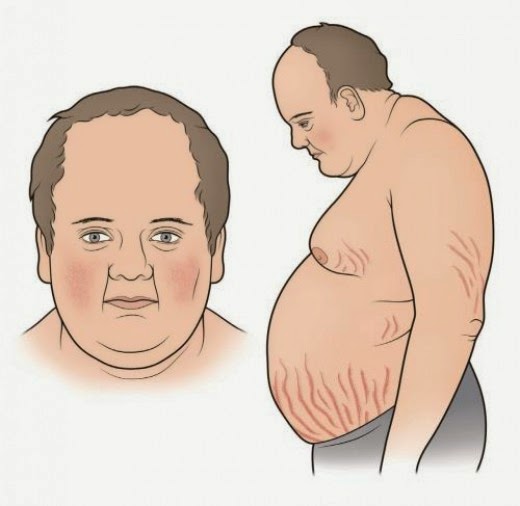
Cushing Syndrome (note that it should not be referred to as Cushing's Syndrome - the possessive form for eponyms is discouraged. Also, the use of eponyms is discouraged) describes the signs and symptoms associated with prolonged cortisol excess of any cause. Cushing Disease specifically refers to cortisol excess due to pituitary stimulation by ACTH. Let's discuss the diagnosis of Cushing Syndrome. First, the presentation of Cushing.
Signs and Symptoms
There are numerous signs and symptoms of Cushings along with a classic appearance:
Diagnosis
Guidelines recommend at least one first line test be performed to diagnose Cushing Syndrome - all of which assess cortisol levels (Endocrine society, 2008). If one of the tests is equivocal or the pre-test probability is high, another one of the first line tests should be performed. First line tests include one of the following:
1. Late night salivary cortisol - Elevated cortisol measurements suggestive of Cushing Syndrome.
2. 24 hr Urinary Free Cortisol - Elevated cortisol measurements suggestive of Cushing Syndrome.
3. Low-dose dexamethason suppression test - Assesses pituitary corticotroph response to steroids. Normal tissue
Once a diagnosis of Cushing Syndrome is established, determing the underlying cause is the next step (ectopic ACTH production vs Pituitary ACTH production vs primary adrenal cortisol excess). Measuring a serum ACTH level is helpful, as it should be suppressed in primary adrenal tumors, but elevated in both ectopic and pituitary sources of Cushing Syndrome.
If serum ACTH is elevated, the next step is to perform a High Dose Dexamethasone Suppression test. Pituitary sources of ACTH excess are only relatively resistant to negative feedack inhibition from glucocorticoid - therefore, with high doses of the potent dexamethasone, suppression of ACTH and therefore cortisol production is expected. However, ectopic sources of ACTH production will not be sensitive to negative feedback, and therefore persistently high cortisol levels are expected. See below.
One last thing...
Who's picture is that at the beginning of the post? That's Peter Cushing, who plays Grand Moff Tarkin in Star Wars: A New Hope (he's the commander of the Death Star). Any relation to Harvey Cushing, the first person to describe the disease? Nope. No relation.
References
Click here for the Endocrine 2008 guidelines on diagnosing Cushing