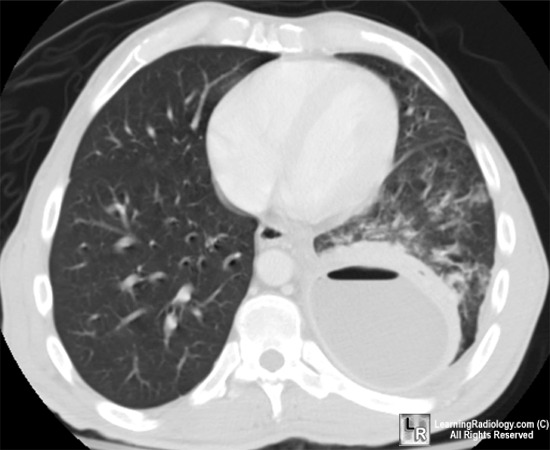
 Today we discussed a patient with a chronic empyema ultimately proven to be secondary to streptococcus anginosus.
Today we discussed a patient with a chronic empyema ultimately proven to be secondary to streptococcus anginosus.Please follow the link to a recent review on parapneumonic effusions and empyema.
Some take-home points about S.anginosus and empyema:
1) The Streptococcus milleri group of organisms is made up of S. intermedius, S. anginosus and S. constellatus which are considered a sub-group of Viridans streptococci. These gram positive cocci are normal flora in the respiratory and GI tract and are known to cause abscesses in the brain, liver, lungs and oropharynx.
2) S.milleri are generally susceptible to beta-lactam antibiotics.
3) In general, lung abscesses related to S. milleri are thought to occur from aspiration of oropharyngeal contents.
4) Don't forget to look for the caramel of butterscotch smell associated with S. anginosus infections! Actually no, please don't.
5) The management includes prompt drainage of any collections and IV antibiotic therapy, usually with a beta-lactam. Duration of treatment is dependent on symptoms, but often a minimum 4 week duration of IV antibiotics is required. Specific antibiotic selection should be based on sensitivity testing.
6) Regarding complicated parapneumonic effusions and empyema:
a) These effusions typically occur in the context of pneumonia and represent a spectrum from an uncomplicated parapneumonic (UPPE) effusion to a complicated parapneumonic effusion (CPPE)to an empyema.
b) The signs and symptoms of an empyema are often indistinguishable from a typical pneumonia. All patients with pneumonia should be assessed for a pleural effusion.
c) In the setting of pneumonia with a pleural effusion, the phrase "never let the sun set on a parapneumonic effusion" is used to emphasize the importance of prompt investigation and drainage if necessary. Effusions greater than 10mm on the lateral decubitus CXR should be sampled.
d) More chronic presentations of an empyema can occur with less virulent organisms such as S.anginosus (as in our patient).
e) In general, a PPE should be drained if the pH of the fluid is less than 7.2, there is a positive gram stain/culture, a glucose less than 40-60 (U.S. units), an LDH greater than 1000 (U.S. units) or the effusion is greater than 50% of the volume of the hemi-thorax.
f) Drainage of a CPPE or empyema typically involves a large bore chest tube +/- adjunctive therapies such as fibrinolytics, VATS or decortication.
we are currently investigating a similar case
ReplyDeletedisturbingly, there is no evidence for aspiration of oropharyngeal contents, despite repeated questioning
has any other possible source for "Strep milleri" pleural empyema been described (I do not have access to the link given...)
best regards,
A. Burnens, MD
head of microbiology labs
Medica, Zurich, Switzerland